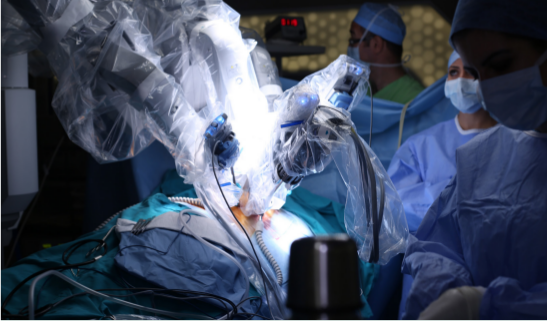
Recent research shows that robotics don’t measure up to advanced laparoscopic techniques when it comes to GYN surgery. While many people assume that a robot is more efficient than a human surgeon, what they don’t realize is that robotic procedures for treating GYN conditions–for example performing hysterectomies–are more costly, require longer operating times, and use a higher number of incisions or ports.
Yet, robots are infiltrating all types of specialties and procedures due to robotics’ companies aggressive marketing to OBGYNs, most of whom only perform surgeries an estimated 20-25% of the time. Robotics are also being taught to OBGYNs in training.
Because many patients inherently trust their OBGYN, if that OB suggests an open or robotic procedure for let’s say a hysterectomy, that patient isn’t going to know there is a better option with a minimally-invasive GYN surgical specialist.
Read more about this issue in Robotics Business Review (page 16).
To schedule an appointment with CIGC surgical specialist Dr. Natalya Danilyants or Dr. Paul MacKoul, call 888-SURGERY or reach out online. Patient feedback is available on our website under Patient Testimonials, and on doctor review sites: Dr. Natalya Danilyants Reviews | Dr. Paul MacKoul Reviews.